Here what he found out:
“One of my patients who is doing well after sleep apnea surgery emailed me a list of all the improvements just a few weeks out, and at the end, just happened to mention that he expects his kidney stones to be eradicated as well.
I didn’t give it much thought, since treating sleep apnea and UARS can help almost anything, but when I went to the literature, I found a study which showed that that sleep apnea can be a direct cause of kidney stones.
What the authors showed was that uric acid excretion by the kidneys is increased in people with kidney stones. After treatment with CPAP, uric acid levels normalized.
This finding is not surprising at all, since obstructive sleep apnea is linked directly or indirectly to almost every chronic medical condition that modern people suffer from.
You would think that all patients who suffer from kidney stones would get screened for obstructive sleep apnea, but as far as I can tell, doctors haven’t changed their thinking about kidney stones at all.
The same thing happened after a study showed that frequent nighttime urination could be cured by treating an underlying sleep-breathing problem. Again, no major changes in the way nocturia and urinary frequency is handled.”
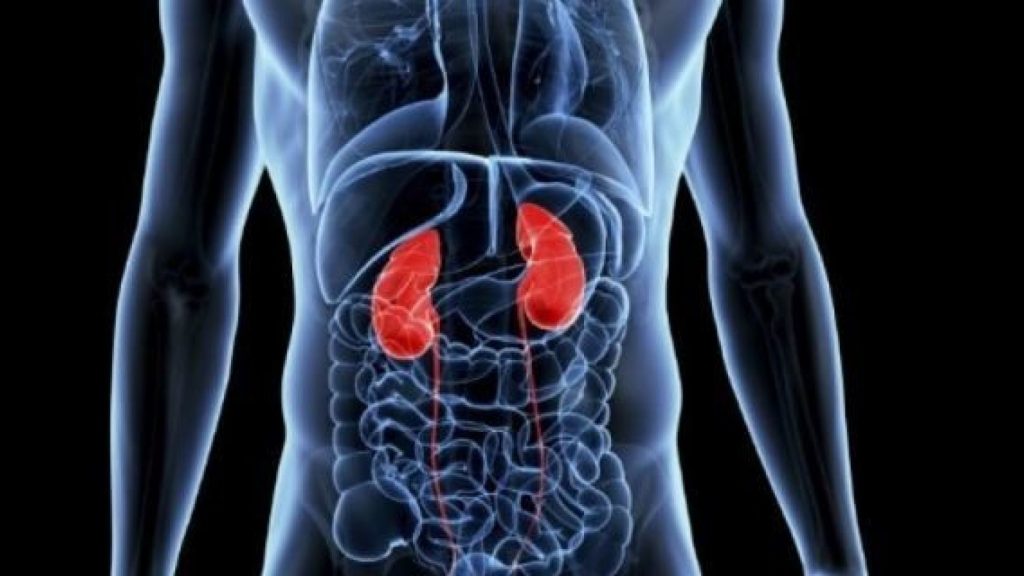
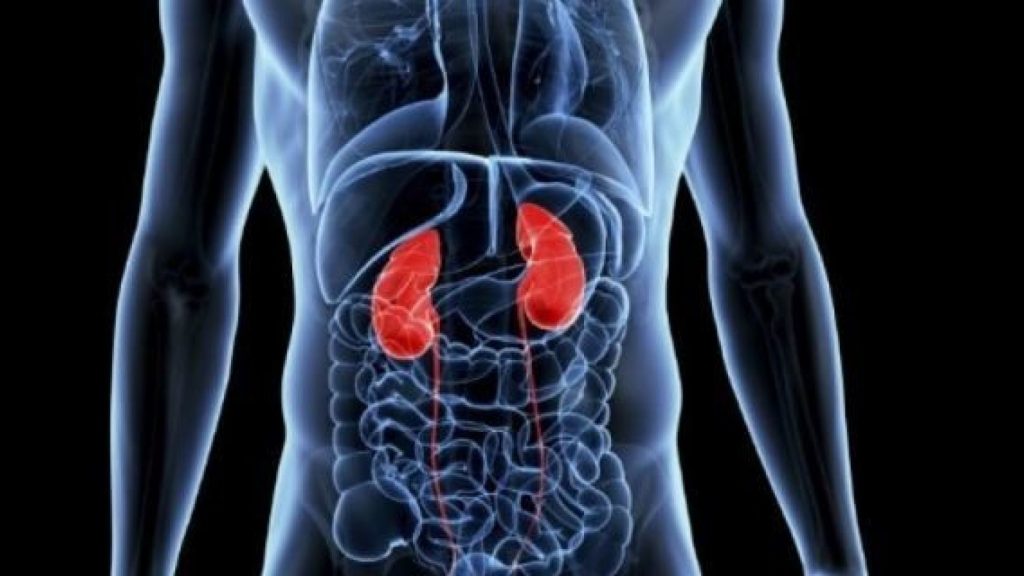
The kidneys are two hard-working organs in the body which can suffer from the long-term consequences of poor sleep. Likewise, kidney dysfunction can negatively affect sleep quality and quantity.
Also, www.sleepapnea.org has published the findings from research into OSA and Kidney health issues here-
The connections between kidney health and sleep health
According to sources at the National Kidney Foundation, as many as 26 million Americans may have un-diagnosed kidney disease.
Because a number of symptoms of underlying kidney disease resemble symptoms of other conditions, it can often be overlooked as the root cause for someone’s health woes. Among those symptoms are those which mirror signs of sleep disorders:
Fatigue, low energy, and inability to concentrate. In kidney disease, the organ less efficiently remove toxins and excess fluids from the bloodstream. This slows down or impairs many physiological systems, including those that support the sleep process.
Fragmented or insufficient sleep. Because of those same impurities in the bloodstream, the body, which relies on balances in hormones and other blood factors, cannot maintain a proper sleep cycle. In addition to insomnia, untreated obstructive sleep apnea can also lead to long-term sleep loss (see below).
The circadian rhythms and kidney function
The kidneys’ ability to metabolize medications and certain nutrients, such as sodium and potassium, changes between day and night due to shifts in our circadian rhythms. Why? The body shifts into a different mode as we sleep, one in which healing can (and should) take place.
However, when we experience poor kidney health, this rejuvenation of the blood doesn’t result in efficient waste filtration by the organs. This can lead to sleep problems.
Dr. Ciaran McMullan of Brigham and Women’s Hospital is a passionate researcher of sleep and its impact on kidney health.
“Kidney function is actually regulated by the sleep-wake cycle,” Dr. McMullan told the National Kidney Foundation last November. “We also know that nocturnal patterns can affect chronic kidney disease and that people who sleep less usually have faster kidney function decline.”

McMullan recently launched new research to study how sleep impacts the kidneys. His particular interest? How melatonin in two forms—endogenous (naturally occurring in the body) and exogenous (in manmade supplemental form)—might influence kidney health and function.
Kidney disease treatment and insomnia: the research
Research published in the August 2008 issue of the American Journal of Kidney Diseases uncovered problems with unchecked insomnia among kidney disease patients using hemodialysis.
Hemodialysis is a critical therapy for those with severe kidney disease. It does the job of removing wastes and excess fluid from the blood when the kidneys fail to do this important work.
More than half, and as much as 80 percent, of patients using maintenance hemodialysis reported problems either with sleeping (waking up too early, problems with waking up and not being able to fall asleep again) or with excessive daytime sleepiness (probably due to fragmented or insufficient nighttime sleep).
The study authors suggest that understanding the way hemodialysis is delivered, along with assisting patients with sleep habits, could help these chronically ill patients to achieve better sleep.
Other research from Canada and the United States also shows a possible connection between hemodialysis and other associated concerns related to insomnia. These include reduced pain threshold and depression.
Secondary Nocturnal Enuresis (SNE) and the sleep apnea connection
More casually known as bedwetting, SNE occurs in adults who usually control bladder function at night, yet experience problems with bladder dysfunction as they sleep.
SNE can be caused by a number of underlying problems. High on the list are snoring and obstructive sleep apnea (OSA). The connection between SNE and untreated OSA was established over 20 years ago.
A Taiwanese study published in 2016 showed substantial evidence for a connection between hypoxemia (a condition of reduced blood oxygen) and injury to the kidneys.
Snoring is also well known as a risk factor for underlying OSA. If a person who snores experiences SNE, it’s likely they will be tested for sleep apnea. Fortunately, treating sleep apnea can resolve the problem of SNE for most people.
Hypertension and diabetes: shared concerns
In both untreated kidney disease and insufficient sleep (by whatever cause), increased blood pressure becomes a common denominator. Uncontrolled high blood pressure can lead to stroke, cardiovascular disease, and aggravation of other health conditions.
One of the kidneys’ chief jobs is to maintain healthy blood pressure. Poor filtration of substances in the blood by the kidneys, however, will eventually lead to hypertension.
Diabetes also joins high blood pressure in establishing confirmed links between poor sleep and kidney dysfunction. Diabetes is the leading cause of kidney disease. One quarter of all diabetics also suffering from poor kidney health.
The kidneys serve a critical endocrine function by supplying the blood with key hormones so that all organs can function properly. Because diabetes involves imbalances in blood glucose, insulin, and certain hormones meant to keep these products in check, the kidneys cannot hope to maintain proper function.
Fortunately, kidney disease caused by diabetes happens slowly over time and can be prevented.
The prevalence of chronic kidney disease (CKD) among people with sleep disorders
Previous cross-sectional research, led by Dr. McMullan and published in Kidney International last June (PDF), also shows that subjects with advanced CKD are more likely to suffer from one or more other sleep disturbances. These include reversals in day-night sleep pattern, trouble falling asleep, broken sleep cycles related to sleep apnea, and/or restless leg syndrome. Sleep deprivation, alone, is proven to result in a decline to kidney function as evidenced by data from the well-known Nurses’ Health Study.
Treating your sleep apnea is vital to your well-being on so many levels. Call Alaska Sleep Clinic today to speak with one of our board-certified sleep specialists.