Sleep loss is a widespread problem, and military veterans are particularly susceptible.
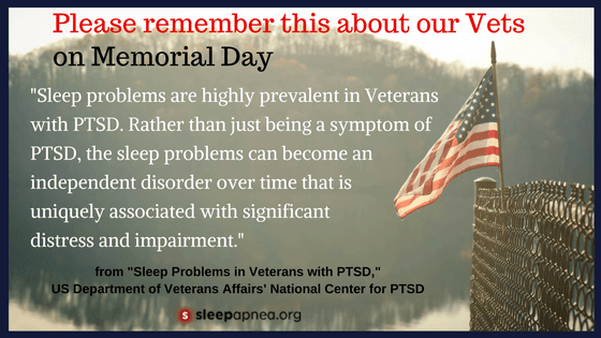
Vets are four times as likely to have obstructive sleep apnea (OSA). In addition, those with Post Traumatic Stress Disorder (PTSD) or a traumatic brain injury have a higher incidence of OSA, meaning that psychiatric and sleep disorders are often linked. Research-based sleep techniques are being developed for those with PTSD, so it’s important to seek specialized help.
Warning signs of sleep trouble:
Sleep troubles can look different depending on the person, but it’s important to seek help if you have warning signs such as,
- Mood symptoms like lack of motivation, depression or anxiety that interfere in work or daily life. Lack of sleep can be both caused by, or a symptom of, a psychological issue.
- PTSD-related symptoms. One of the hallmarks of PTSD is difficulty sleeping, as well as nightmares and flashbacks. Insomnia can be a symptom of PTSD, or a separate issue on its own.
- Excessive sleepiness. Everyone has the occasional drowsy day, but if sleepiness is common for you, or you need many catnaps during the day, you may not be getting the amount or quality of sleep you need.
- Sleep disorder symptoms. Having trouble falling asleep or staying asleep, snoring, feeling tired during the day despite having slept enough at night—these may be related to a sleep disorder. Veterans have higher incidence of obstructive sleep apnea, so it’s important to be aware of daytime drowsiness, interrupted sleep, or breathing troubles at night.
How to get better sleep.
You don’t have to live with sub-par sleep, and in fact letting a sleep disorder go untreated can be dangerous to your health or the safety of those around you. If you suspect a sleep problem, talk to your doctor and also learn more about sleep hygiene.
- Eat well and exercise. Regular activity and meals that center around vegetables—this will lower stress and improve sleep. Go outside in the daytime to help regulate your internal clock. Avoid alcohol and smoking before bed.
- Practice good sleep hygiene. Go to bed and wake up at the same time every day. Your bedroom should be dark, cool, and quiet.
- Manage your stress. Find a book or podcast to teach you simple mediation practices. These can be very powerful, as they clear your mind of worries and allow you to relax. Veterans are known to be on “high alert” long after they return from duty, so regular mindfulness or meditation can be an important practice.
- Talk to a therapist. Mood symptoms like anxiety and depression can make it hard to sleep, but lack of sleep can also worsen emotional struggles, so the cycle feeds itself. Find a specialist in sleep disorders, and specifically one trained to help veterans. There are evidence-based treatments available that tailor cognitive behavioral therapy methods, helping those with PTSD to improve sleep.
- Consult with your doctor. Ask for a referral to a sleep medicine specialist. In conjunction with sleep hygiene changes and therapy, you may benefit from sleep medications or treatment for disorders like sleep apnea.
The health of our military members is our collective responsibility and concern. Their sleep must not be overlooked as a critical component of their health and wellness, both during the time of active service and for the duration of their lives. We honor our soldiers when we care for them, and that includes caring for—and about—their sleep.
Soldiers and Veterans are of the highest concern to all of us here at Alaska Sleep Clinic. If you or a loved one has any sleep-related issues mentioned in this article, do not hesitate to call us for your free sleep assessment.
Alaska Sleep Clinic is proud to be the ONLY Veteran-Owned Small Business Sleep Clinic in Alaska.