If a good night’s sleep helps the brain and body perform better, it’s a good guess that sleep problems can cause more than just fatigue. Numerous studies have shown a connection between sleep disorders and medical conditions such as cardiovascular disease, cerebrovascular disease, and metabolic disorders, including the risk of obesity and diabetes. Now researchers outline several interesting associations between sleep disorders and eye disease.
Obstructive sleep apnea and eye disorders
In the November year issue of Mayo Clinic Proceedings, Mayo Clinic researchers outline several interesting associations between sleep disorders and eye disease.
More than 12 million people in the United States have obstructive sleep apnea — a potentially serious sleep disorder in which breathing repeatedly stops and starts during sleep. Sleep apnea has several types. The most common is obstructive sleep apnea (OSA), which occurs when throat muscles relax and block the airway.
Multiple studies have identified OSA as an independent risk factor for the development of several medical conditions, including high blood pressure, which are related to impairments or alterations in a person’s vascular (circulatory) system. With their own complex and sensitive vascular system, the eyes can sometimes signal and be affected by systemic vascular problems.
“Given the vascular consequences of OSA, it is not surprising that ophthalmic manifestations exist,” explains the article’s lead author, E. Andrew Waller, M.D., a Mayo Clinic pulmonologist and sleep specialist.
The researchers conducted a literature search focused on sleep disorders and eye disease. In the article, they discuss a variety of ophthalmic conditions associated with obstructive sleep apnea.
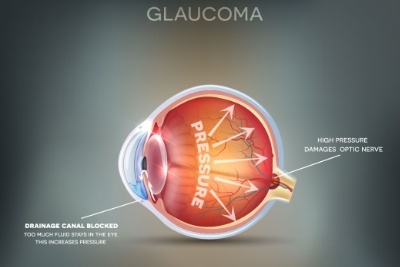
Sleep Apnea and Glaucoma
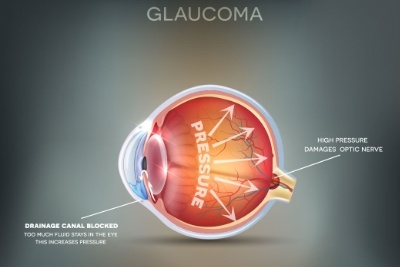
Glaucoma is the second most common cause of blindness and the most common cause of irreversible blindness. Obstructive Sleep Apnea is linked to two forms of this disease — primary open-angle glaucoma (POAG) and normal-tension glaucoma (NTG). The severity of glaucoma appears to correlate with the number and duration of apnea episodes in patients with OSA.
Glaucoma, which can be several optic nerve damaging eye conditions, is typically caused by high pressure within the eye, according to the Mayo Clinic. Symptoms are usually slow-progressing, with vision loss being one of the only signs. Certain risk factors like a patient’s age are well known; while ones like ethnicity are less known by the public.
A number of clinical studies over the last several years have shown an association between sleep apnea and several glaucoma indicators such as intraocular pressure (IOP), visual field mean deviation, cup-to-disk ratios, and retinal nerve fiber layer thickness.
There have been a number of studies showing the reduction in IOP among glaucoma patients following use of a CPAP machine. Still, the complexities of glaucoma as well as the wide variations in OSA severities make a direct correlation more elusive. Some studies have suggested that CPAP therapy can even raise IOP to some degree, but many researchers generally agree that the risk is possible in a smaller subset of OSA patients.
Even then, most researchers and medical experts see the increased oxygen levels attained through use of CPAP and the overall health benefits far outweighing the hypothetical risks. The takeaway for OSA patients, especially those with severe forms of the condition, is to work with their physician and sleep therapist to monitor all physiological conditions and ask questions.
How is floppy eyelid syndrome related to sleep apnea?
This disorder causes eyelids to evert (turn inside-out) spontaneously during sleep, resulting in excessive watering, stickiness, discomfort and blurred vision. While not a serious medical problem, this syndrome can signal that a person also has OSA, which can lead to more significant health problems.
A 2010 study looked at 102 patients with FES and a control group of another 102 patients. 90% of study participants with FES also had obstructive sleep apnea.
Researchers aren’t exactly sure why. In addition to shared risk factors (obesity, age), it could be that those with OSA have greater tissue elasticity which also affects incidence of FES.
According to Dr. Brad Sutton, OD, FAAO, of the Indiana University School of Optometry, “The incidence of sleep apnea in patients with floppy eyelid syndrome (FES) is essentially 100%.” Dr. Sutton urges his patients with FES to get tested for sleep apnea. FES is often treated as eye irritation with drops before the patients are properly diagnosed. However, finding out if the patient has sleep apnea and then treating the sleep apnea is the best approach as this will likely improve the FES.
Dr. Sutton’s treatment approach is three parts:
- *Using a thick lubricating ointment at night.
- *Sleeping with a cylindrical pillow to minimize contact with the eye and the pillow at night.
- *Wearing a firm sleep mask or taping the eyelids down to prevent eversion (flipping).
If those treatments don’t work, surgery to tighten the eyelid tissue may be required.
Non-arteritic anterior is chemicoptic neuropathy (NAION)
Research shows an increased incidence of OSA in people diagnosed with NAION. This condition is characterized by the sudden painless onset of vision loss in one eye, often noticed upon awakening. Up to 6,000 patients annually in the United States are diagnosed with this condition, which can cause irreversible vision loss.
Papilledema
People with OSA may have a higher incidence of papilledema, swelling of the optic nerve in both eyes. Papilledema typically occurs due to increased pressure within the skull and can lead to progressively worsening vision and, in some cases, blindness.
Healthy Eyes and Healthy Sleep
Russell Beach, O.D., who practices in Virginia, notes that ocular health issues—including floppy eyelid syndrome and normal-tension glaucoma—may be common in sleep apnea patients. Floppy eyelid syndrome can lead to eyelids that don’t provide effective protection for the eyes during sleep, which can cause dryness, severe ocular surface disease and even corneal abrasions. Glaucoma is also often linked to sleep apnea because the disorder affects the amount of oxygen being transported to end organs; when oxygen concentration to the optic nerve is reduced, the nerve becomes susceptible to damage.
Dr. Beach also recognizes CPAP machines can have an effect on a person’s eyes. Dr. Beach is in a unique position to discuss the effects of sleep apnea on eye health, because he has sleep apnea himself.
Depending on the severity of the apnea events, the condition can be life threatening and the CPAP machine greatly reduces those risks, so it should not be discontinued due to ocular irritation. Instead, the mainstay of treatment has to be protecting the ocular surface. The most efficient way to do this is to instill thicker artificial tears just prior to bedtime. Gels and ointment artificial tears should be considered.
Alaska sleep Clinic works closely with some local ophthalmologists to learn more about the connection between sleep apnea and eye disease. Watch the KTUU Channel 2’s “Moms Everyday” segment with Dr. Sherry Lentfer from Katmai Eye below.
https://www.facebook.com/plugins/video.php?href=https%3A%2F%2Fwww.facebook.com%2FAlaskaSleepClinic%2Fvideos%2F1758570414203434%2F&show_text=0&width=560

Story Source:
Materials provided by Mayo Clinic. The authors from Mayo Clinic are Rick Bendel, M.D., ophthalmologist and Joseph Kaplan, M.D., pulmonologist and sleep specialist.
www.thecpapashop.com. The author Chris Vasta.
www.emedicine.medscape.com. Author Mark Ventocilla, OD, FAAO
Note: Content may be edited for style and length.